Many health system leaders are developing health equity plans to participate in new value-based care payment models. The new ACO REACH payment model from the Center for Medicare and Medicaid Innovation (CMMI) has increased these efforts.
It may seem reasonable to repurpose annual Community Needs Assessments (CNA), or Impact reports to be compliant with the new regulations. Doing so, however, misconstrues the CMS’ wording and intent and may lead to additional regulatory scrutiny and potential payment reductions. Pleas of confusion over vague CMS wording hasn’t stopped them from levying fines. CMS has issued fines for lack of compliance with new price transparency regulations despite perceived lack of clarity and intent. It would not surprise us to see similar penalties for health equity plans that repurpose Community Needs Assessments.
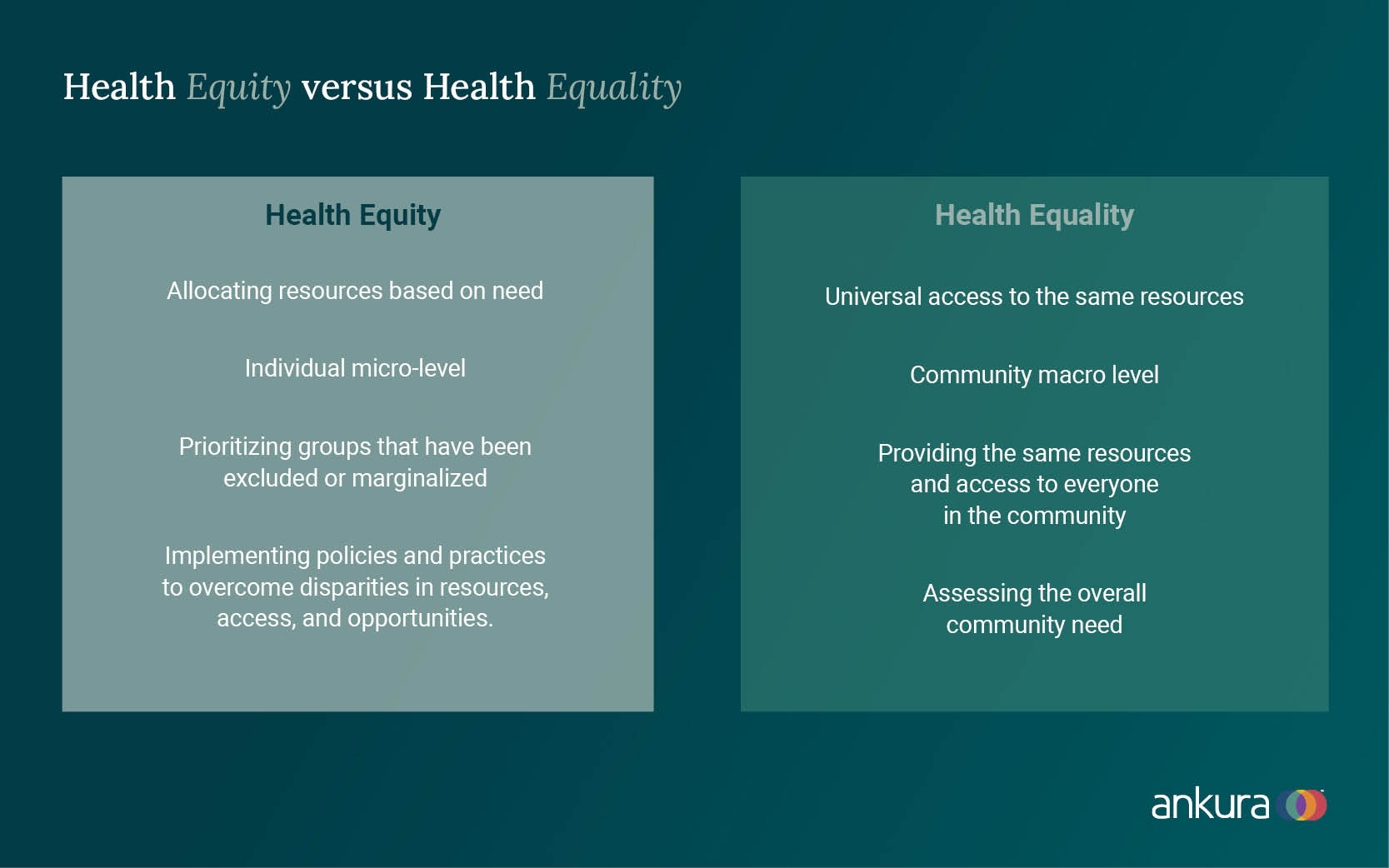
Health equity versus. equality: why the difference matters
The terms health equity and health equality are often used interchangeably but mean different things. The Robert Wood Johnson Foundation (RWJF) provides the following definition of health equity:
“Health equity means that everyone has a fair and just opportunity to be as healthy as possible. This requires removing obstacles to health such as poverty, discrimination, and their consequences, including powerlessness and lack of access to good jobs with fair pay, quality education and housing, safe environments, and health care.”
Health equity plans address inequities in the ability of people to access care. These plans require a granular evaluation to find gaps in individual health needs. Health equity plans may require allocating resources differently to achieve an equal outcome.
In contrast, health equality provides the same resources to everyone regardless of circumstance. Because CNA reports focus on health equality, they miss that underserved groups may need extra resources. This overlooks the intent of CMS to mitigate health disparities. To ensure health equity, those in poor health and who have fewer resources, need more efforts dedicated to improving their health. This may be quite different than the typical challenged community or someone caught up in the opioid epidemic.
Despite having access to the same resources, disadvantaged individuals often have worse health outcomes. Lack of control, respect, and money arise from the foundations of our society. The consequences of this inequity are apparent in state or national statistics like life expectancy or cost of housing but are also based on local communities / cultures and individual situations. Common health disparities include insufficient health insurance, limited access to care, the burden of disease, and mental health challenges.
Vantage Health Technologies recently surveyed healthcare executives and found that the majority believe health equity is important, but that nearly half have no roadmap to address those issues. Key highlights from the survey include that 48.3% of survey respondents say they don’t know if they have race, ethnicity, or language data on their care population, while 44.3% of respondents say they only provide care in English.
Merge micro and macro views to understand individual health needs
Inequity is harder to see from a birds’ eye view. On a community-wide macro scale, small numbers average out with larger numbers. But individual interactions, qualitative survey feedback, and ethnographic research reveal a different story on a micro scale.
To develop an effective health equity plan, merging the macro view with the micro view is a better way to improve individual patient outcomes. Now that technology gives us the ability to analyze massive quantities of data (through patient wearables and portals that coordinate care across multiple providers) we can look at one person at a time, aggregated as whole. This is our best hope to help entire communities wipe out health disparities and close gaps in health equality at an individual level.
Better data helps you make a bigger impact
Querying national and state demographic statistics will only yield health information at the zip code or block level. You must have access to robust community and provider based (EMR and claims) data sets if you intend to truly advance personal health. These enable you to zoom in to subsets of individuals with similar social / economic behaviors and circumstances.
These subsets may show a particular suburban area of your market. Or a group of individuals who share similar health indicators such as diabetes. Or employees who work in a distribution center.
Five components of a robust health equity plan
To create and execute a true health equity plan, we recommend including the following components.
Identify and prioritize health disparities. There are many disparities in health that are related to opportunity and resources. Increasing opportunities benefits everyone. But prioritizing and focusing on groups that have been excluded or marginalized should be at the top of your list. Start by analyzing and prioritizing those whose outcomes are significantly worse than others. Once you pinpoint these individuals, consider strategies to significantly reduce the contributing factors. As an example, one place to look is at your inpatient admissions. Based on their diagnoses, who shouldn’t be there? Or more importantly, who had a length of stay outside the norm and why?
Plan to make structural programmatic changes. What sets health equity plans apart from community health assessments is their focus on changing and implementing policies, laws, systems, environments, and practices to reduce inequalities in resources, access, and opportunities. Concentrate on eliminating unfair individual and institutional conditions that create inequities rather than assessing the overall community need. One place to start is by looking at your local community organizations, employers, and governmental resources. Is there a coordinated system of communication and shared resources? Are their policies and procedures similar? Why does one subset of the community use one resource more heavily than another? Lead with probing questions and then listen for structural similarities or differences to understand local community dynamics.
Determine your model for implementation. This may be a new delivery model for your organization or a modification of an existing one. How does focusing on equity change our approach to patients? For instance, partnering your in-house dietary resources with a local food bank to ensure continuity of diabetic dietary guidelines is a way to coordinate care outside traditional methods of education. What outcomes would you measure for your diabetic frequent flyers? How would this change how and whom you are recruiting? How do we expect to be compensated?
Solicit help and partners in your plan. Health disparities aren't just a provider challenge – also a community one. Look for ways to engage safety net providers, FQHCs (Federally Qualified Health Centers), rural health clinics, and behavioral health providers. Enlarge your network of partners to help tackle root cause issues at the individual level. For instance, Novant Health is partnering with Charlotte Mecklenburg Library to provide health screenings and health services navigation in the underserved Hickory Grove and West Boulevard communities. Dedicated on-site health workers will connect citizens to housing, food, and primary care. Regularly scheduled visits from the mobile unit will provide health screenings and immunization events for under- or uninsured children.
Play the long game. The key to reducing health disparities is consistency. Plan for consistent evaluation, focus on what is working and what is not, and monitor short and long-term metrics. Consistently compare the disadvantaged to the advantaged, not the overall general community. Progress may take decades or generations to realize positive outcomes, but advancement is only realized with consistency.
Know whom you are trying to help. Do not just assume that the data tells you everything you need to know. Actively engage your constituents in the identification, design, implementation, and evaluation of your proposed plans.
In seeking strategies to impact health disparities, sometimes the needs are so widespread that it is tempting to stand farther and farther back to comprehend the full view. We challenge you to also zoom in and look for bite-sized and achievable ways to make a meaningful difference in righting the scales. A recent piece in Harvard Business Review describing how SCAN Health Plan reduced disparities demonstrates how narrowing the focus to a specific issue can yield faster results.
Innovation comes from stepping forward. Resist repurposing your Community Needs Assessment or Impact Reports. Challenge your organization to start anew. Who knows ...you might just change lives!
© Copyright 2022. The views expressed herein are those of the author(s) and not necessarily the views of Ankura Consulting Group, LLC., its management, its subsidiaries, its affiliates, or its other professionals. Ankura is not a law firm and cannot provide legal advice.



