Every day the news publicizes healthcare industry challenges. However, we must counter the doom-and-gloom mentality by focusing on variables within our control. Approaching these variables with a Charles Darwin mindset, “it is not the strongest of the species that survives, nor the most intelligent, but the one most responsive to change,” will lead us to think differently about how we manage future operational costs.
The following cost-reduction tactics are achievable for any leader to implement once they overcome the mental hurdle of making a change.
1. Five Ways to Contain Healthcare Labor Costs
When labor costs are nearly 500% higher than pre-pandemic levels and projections show an $86B increase in 2022 alone, there is an urgent need for change. We recommend that providers evaluate their labor cost strategies by considering the following:
Reduce turnover costs by offering customized benefits based on life stage
With the average RN (Registered Nurse) turnover cost hovering around $40,000, retaining existing staff is a tremendously impactful way to save money. One strategy to retain a multi-generational workforce is to tailor benefits packages to align with employees’ life stages. Organizations can do this by offering “longevity pay” for tenured employees to retain highly experienced staff in middle management. Longevity pay also helps retain entry-level staff who have capped out their pay grade but provide significant value to the organization.
Another life-stage-specific benefit is to offer parental leave and subsidized childcare for those in an early to mid-career phase. Likewise, one could offer dependent or elderly care for seasoned team members. Logistically you may offer these benefits to everyone, but the differentiator is in the packaging and timing of them at opportune moments. While the choice to vary benefits within an organization is a change mindset hurdle to surmount, the cost of offering enhanced benefits to retain existing staff is significantly lower than a turnover or hiring contract labor.
Generate more revenue by leveraging clinical assistants and medical techs at a higher frequency
Reintroducing “team nursing” or revisiting your team nursing strategy will allow staff to work closer to their top of license by leveraging clinical assistants and medical techs at higher rates. For instance, if you are short-staffed on RN coverage, pairing them with LPNs or MAs will enable them to manage their time based on acuity, resulting in RN direct patient care hour increases for those who are sicker, while the team can help to cover less acute patients. This not only increases nursing satisfaction but also productivity in areas that enhance patient outcomes.

Use technology to trim inefficient staffing based on real-time needs
Implementing scheduling technology to manage and enforce accountability provides greater capacity to adapt staffing models based on real-time conditions. Understanding the nuances between projected versus actual resource needs and the variance between the two allows management to continuously improve their costs and close the gap in inefficiencies. Also, pay-to-punch realities (example: clocking in early and leaving late to capture overtime) are allowing hourly employees to create labor waste. If managed effectively, the cost savings can equate to hundreds of thousands of dollars each year. For the registered nurse population in one of our clients’ markets, the savings equated to as much as $300K per year. The cost savings are real, but you can’t manage what you aren’t measuring.
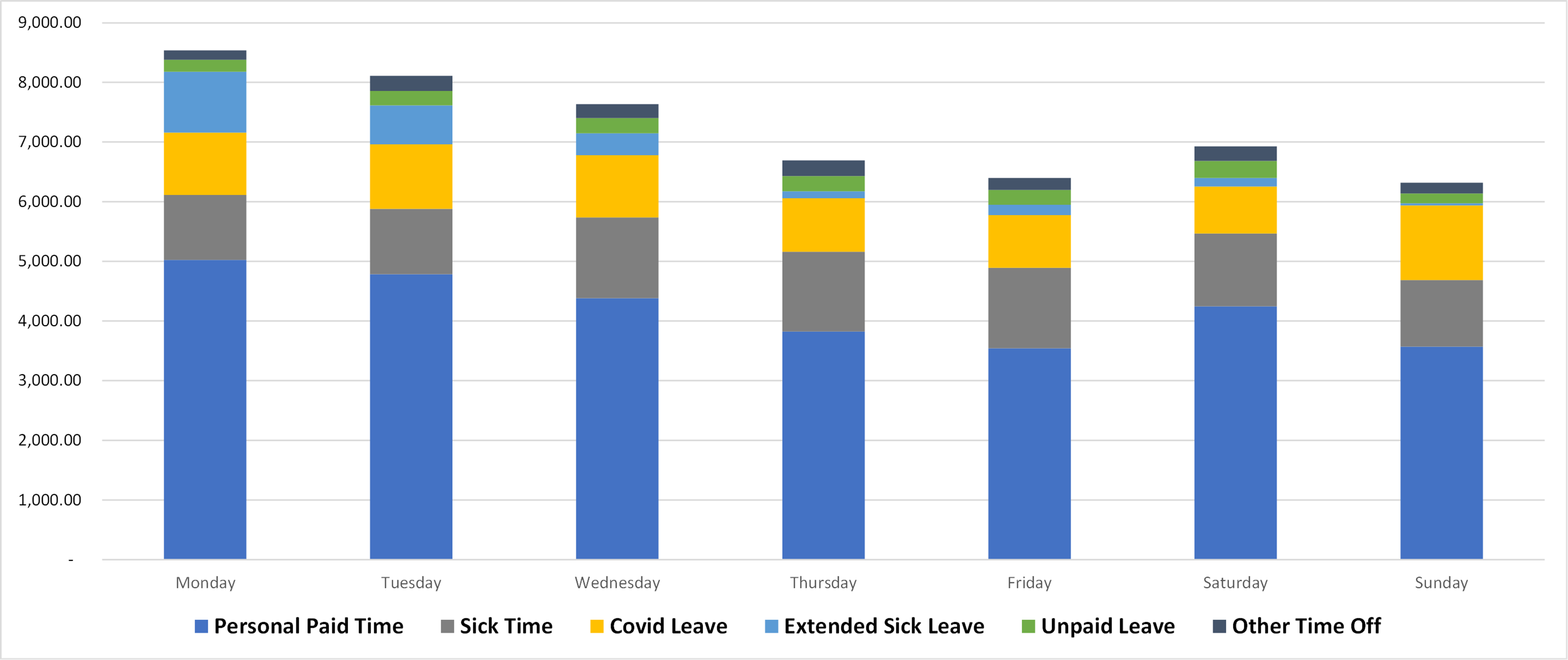
Using Data to Make Staffing Decisions
This chart shows how we measure staff call-outs by the day of the week. Data analysis enables us to assess the situation and start to ask questions about why Mondays have the highest number of callouts. Once supervisors understand the reasons why they can develop solutions and incentives to make staffing less variable and prevent staff shortages.
Convert contract labor to permanent FTEs (Full Time Employee) to cut inefficiency and turnover costs
The current workforce shortage and increased contract rates based on demand have elevated labor costs to unsustainable levels. Yet the long-term cost to the organization isn’t really in the contract rates but in the consistent turnover of team members, the lack of standardization, the inconsistent team dynamics, and the brain drain of experience and historical knowledge. Culturally, high usage of contract labor is like a virus that slowly degrades the organization’s core foundations. A multi-pronged strategy that starts with retention and ends with converting contract staff to permanent FTEs is vital to the long-term stability of healthcare organizations.
Seek unconventional sources of permanent FTEs to reduce dependency on expensive contract labor
Recruitment strategies to secure a supply of incoming staff must become more creative. Building partnerships with local schools is a natural talent pipeline. Also, hospitals are recruiting highly skilled international nurses who offer the added benefit of affinity with a diverse patient population. Welcoming back and celebrating “boomerang” employees has been another successful recruitment strategy.
Renegotiating agency contracts, looking for alternative sources of staff, deploying a top-of-license team approach, and streamlining process inefficiencies to increase productivity are just a few of the current strategies being deployed to gain a permanent workforce. There are no quick fixes.
2. Conserve Costs by Combating Hospital Use Rate Plateaus with Efficient Operations
While the shift to value-based payment has started, volume still drives revenue. And since many providers haven’t seen volumes surpass pre-pandemic numbers yet, hospital revenue is suffering. Despite beliefs that volume and use rate trends will bounce back, COVID rapidly taught the public how to access more convenient, affordable options for outpatient care. Consequently, hospital-based use rates have plateaued.
Now, providers have lower volume and higher acuity inpatients that require more resources (at higher costs) and longer lengths of stay, resulting in lower margins. Reallocating resources based on volumes and acuity (CMI) helps combat use rate plateaus in a fee-for-service financial model.
Tactics for reallocating resources include real-time staffing adjustments, infrastructure flexibility with multi-purpose functions, and aggressive caregiver training and education. The organization’s ability to flex up and down based on volume and acuity will help to reduce overall fixed and variable cost structures while continuing to provide patients with an optimized experience and outcomes. While ultimately the system will need to capture additional market share to grow use rates, efficient operations are a faster-to-implement strategy within your realm of control today.
3. Reduce Costs by Trimming Underutilized Services
For decades, community providers have straddled investing in a known identity (cancer, stroke, CV, pediatrics, etc.) with investing in the ability to treat every condition that could present in the ED (Emergency Department). The effect has been to dilute the investment across everything without capitalizing on a particular specialty or becoming a unique destination. In essence, the definition of a commodity. The financial ramification of this approach is a loaded fixed cost structure that has very little margin for variability or nimbleness. This manifests in a heavy healthcare real estate and corporate overhead burden.
The solution is to conduct a cost/benefit analysis on each service offering across all geographical locations. Identifying niche services and programs based on service line excellence or population demographics (geriatric, women, and so forth) will shift providers out of the “jack of all trades” mindset and help build brand reputation capital.
Where possible, we recommend that providers reduce duplication of services, consolidate programs across networks, and operationally right-size or eliminate programs that do not meet clinical efficiencies or economies of scale to justify continued viability. These strategies assist in streamlining operational costs based on margin, but more importantly, provide efficient care at a lower cost. Moreover, systems that have built strong brand awareness around specific service line expertise can create destination centers and save money through reputation capital.
Providers also can develop robust call/transfer centers to promote continuity of care and maximize capacity across the system. These transfer centers help distribute patient visits and volume across the system on a real-time basis, which leverages the fixed cost structure, reduces patient wait times, and maximizes provider productivity. These transfer centers match appropriate services to the patient’s condition, reduce the time to treatment, and optimize clinical outcomes.
4. Reduce Costs by Shortening Throughput
There is a significant opportunity to save money in day-to-day operations and patient throughput by scheduling based on real-time volume and directing referrals based on capacity and predictive behaviors. However, this requires investment in EHR (Electronic Health Records) and data technology. Again, you can’t change what you don’t measure. Once providers put strong systems in place and establish target metrics, then management has a clearer picture of the system goals and can build processes to achieve those cost reduction targets.
The fluidity of contract and traveler staff can make tracking data and maintaining target goals a challenge. Therefore, we recommend implementing practices such as immediate rooming in the ED and leveraging Express Admit Units to reduce the patient’s overall length of stay.
A well-orchestrated case management program aligns care with the right cost structure (location, bed, staffing, etc.), reduces Length of Stay (LOS) through appropriate discharge planning, and enables timely physician decision-making.
Tactics to shorten Length of Stay include:
Eliminate Manual and Redundant Processes
Provide and Ensure Post-Acute Contact Information & Accuracy
Specific Discharge Protocols and Staff and Accountability
Provide Post-Discharge Transportation Options
Accessing Real-Time Post-Acute Capacity and Bed Availability
Managing Patient Expectations and Choices
Triaging Preventative Care and Appropriate Admissions
These strategies have become especially important as we have seen Length of Stay steadily rise post-COVID along with associated resource costs.
CONCLUSION
Despite the “doom and gloom” of the news headlines, we have the power to choose our response. We can identify the major cost outliers and formulate strategies to reduce our exposure. We believe these quick strategies, as well as the longer-term ones, will move the needle in the right direction with commitment and intention no matter the fiscal environment.

Want to know more? Follow Erin Nelson and Michelle Mader on LinkedIn to stay abreast of their latest healthcare strategy insights.
About Ankura Healthcare Real Estate Strategy and Solutions
Ankura multi-disciplinary teams partner with healthcare organizations to align facility resources with care delivery strategies. As the industry undergoes rapid transformation, we help you adapt to regulatory uncertainty, shifting reimbursement models, and economic volatility. Today’s investment strategies address new care delivery models, disruptive market entrants, and digital health change.
Ankura helps you manage costs and risks to ensure that your investment realizes its financial value to the organization today, as well as decades into the future.
© Copyright 2022. The views expressed herein are those of the author(s) and not necessarily the views of Ankura Consulting Group, LLC., its management, its subsidiaries, its affiliates, or its other professionals. Ankura is not a law firm and cannot provide legal advice.




